Your guide to how what might be causing your knee pain and how Physioactive can help.
Physioactive has a knee rehabilitation program for you. From our high-performance program for aspiring young athletes and our professional athletes to our return to sport and daily life for our active adults to our post-operative program be it post ACL repair or meniscectomy, or our total joint replacement rehabilitation program we have the perfect knee program for you. Many of our semi-pro and professional athletes move from our post-op program into our high-performance program here at Physioactive. Led by our knee program director, we will accurately assess your needs and tailor your knee rehab to your age, stage, and goals.
What Physioactive can do for you and your knee injury?
Physioactive believes that full restoration of mobility, stability, and control, and ultimately confidence in your knee is essential for a return to sport and everyday life. Whether it is an acute injury from a twist or if your knee just started hurting our highly trained professionals will be able to accurately diagnose your condition and find out why it occurred in the first place. Along with our skilled practitioners, we have the latest technology to enhance the healing process. Knee pain is a very common musculoskeletal complaint that clients seek help for at Physioactive. As our society becomes more active, the number of knee problems is increasing. Knee pain has a wide variety of causes and treatments.
Get to know your knee and why it might be hurting.
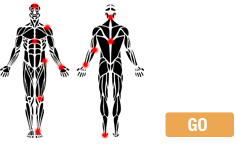
Anatomy of the Knee
The knee joint’s main function is to bend and straighten, as well as bear the weight of the body along with the ankles and hips. We evolved from walking on all fours so these joints take on more force than their original design intended. The knee also twists and rotates. In order to perform all of these actions and to support the entire body while doing so, the knee relies on a number of structures including bones, ligaments, tendons, and cartilage.
Bones
- The knee joint involves 4 bones. It is mainly considered to be the joint between your thigh bone (femur) at the top connecting to the shin bone in the lower leg (or calf area), the tibia, providing the bottom weight-bearing portion of the joint.
- The kneecap or patella rides along the front of the femur.
- The remaining bone in the calf and shin, the fibula, is not truly involved in the weight-bearing portion of the knee joint. It provides ligament attachments for stability.
Ligaments
- Ligaments are dense fibrous bands of connective tissue that connect bones to each other.
- The knee includes 4 important ligaments, all of which connect the femur to the tibia:
- The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) provide front and back (anterior and posterior) and rotational stability to the knee.
- The medial collateral ligament (MCL) and lateral collateral ligament (LCL) located along the inner (medial) and outer (lateral) sides of the knee provide medial and lateral stability to the knee.
Tendons
- Tendons are fibrous bands that attach muscles to bones..
- The 2 important tendons in the knee are (1) the quadriceps tendon that connects the quadriceps muscle (actually 4 muscles, hence “quad”), which lies on the front of the thigh, to the patella and (2) the patellar tendon connecting the patella to the tibia (technically this is a ligament because it connects 2 bones).
- The quadriceps and patellar tendons are sometimes called the extensor mechanism, and together with the quadriceps muscle, they facilitate leg extension (straightening).
- Your knee has 3 hamstring tendons that can be felt on the back of your knee, 2 on the inside and one on the outside of the knee.
Cartilage
- It is the smooth covering on the bones of a joint to allow smooth, near-frictionless movement of a joint. The knees have a cartilaginous thickening called menisci (one is a meniscus) that lie on the top of the tibia and lie between the tibia and the 2 knuckles at the bottom of the femur (called the femoral condyles). The menisci’s primary job is to provide shock absorption for the knee joint.
Bursae
- Bursae are fluid-filled sacs that help to cushion the knee. The knee contains 3 important groups of bursae:
- The prepatellar bursa lies in front of the patella.
- The pes anserine bursa is located on the inner side of the knee about 2 inches below the joint.
- The infrapatellar bursae are located underneath the patella.
Home Care for Knee Pain
Inflammation is the body’s own physiological response to an injury. It begins the healing process. In treating many types of knee pain, a common goal is to break the inflammatory cycle. The inflammatory cycle starts immediately after the injury. We often tell our clients that our bodies have a terrific ‘ON’ switch, but don’t always have the best “OFF” switch. This is where PhysioActive therapy can help. After an injury, substances that cause inflammation invade the knee, which causes further injury, which leads to further inflammation, and so on. This cycle of inflammation leads to continued or progressive knee pain. Although inflammation is the key to healing, controlling the degree of inflammation is imperative. The cycle of pain can be broken and the speed of repair can be improved.
Some common home care techniques for knee pain that control inflammation and help to break the inflammatory cycle are protection, rest, ice, compression, and elevation. This regimen is summarized by the memory device PRICE.
PROTECT the knee from further trauma.
- This can be done with knee padding or splinting.
- A pad over the kneecap, for example, helps to control the symptoms of some knee injuries (an example is a form of bursitis sometimes called housemaid’s knee) by preventing further repetitive injury to the prepatellar bursae.
REST the knee.
- Rest reduces the repetitive strain placed on the knee by activity.
- Rest both give the knee time to heal and helps to prevent further injury.
ICE the knee.
- Icing the knee reduces swelling and can be used for both acute and chronic knee injuries.
- Most authorities recommend icing the knee 2 to 3 times a day for 20-30 minutes each time.
- Use an ice bag or a bag of frozen vegetables placed on the knee.
COMPRESS the knee with a knee brace or wrap.
- Compression helps to accomplish two goals:
- First, compression is another way to reduce swelling.
- Second, in some knee injuries, compression can be used to keep the patella aligned and to keep joint mechanics intact.
ELEVATE the knee.
- Elevation also helps reduce swelling.
- Elevation works with gravity to help fluid that would otherwise accumulate in the knee flow back to the central circulation.
- Prop your leg up when you are sitting, or use a recliner, which naturally elevates the legs. Elevation works best when the knee — or any other injured body part — is higher than the level of the heart.
Over-the-counter pain medicine: Commonly used pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAID’s) like naproxen (Aleve) and ibuprofen (Advil or Motrin), can play a role in the treatment of knee pain. At Physioactive, we will work with your physician to maximize your recovery.
- These drugs directly control pain and, at higher doses, act as anti-inflammatory agents, helping to break the inflammatory cycle. Like all medications, however, these drugs have side effects. We do our best to treat our clients as soon as possible to minimize the need for medications.
- You should not use NSAIDs if you have a problem with bleeding or stomach ulcers and some types of kidney disease, but this must be discussed with your doctor.
When you are deciding whether to call the doctor about your knee pain, a good rule of thumb exists for most long-term knee injuries. If your symptoms have not gone away after trying a week of PRICE therapy you should set up an appointment with your physiotherapist or doctor or a sports medicine or orthopaedic (bone and muscle) specialist to further evaluate the pain. This rule can also be applied to new knee injuries that are not disabling. Remember, however, that this rule should only serve as a guide. If you are concerned about the pain, you should call the doctor.
When should I go to the Hospital for Knee Pain?
If you cannot put weight on your knee, you should consider going to the ER to be evaluated by a doctor because of the possibility of a fracture.
- Many fractures may require immobilization in a specific position or surgery.
- Putting off seeing a Physiotherapist or doctor may hinder healing.
Other signs and symptoms that demand emergency evaluation:
- Fever (which may indicate infection)
- Unbearable pain
- Large wounds
- Puncture wounds
Swelling, if you are on a blood thinner such as Coumadin or have a bleeding disorder such as hemophilia.
What to expect from your assessment of your knee: The Physioactive difference
History: Even in today’s world of technology, our therapists rely on a detailed history and physical exam more than any single test. A clinical exam will give you a more accurate diagnosis than most MRI’s.
Your therapist will typically want to know the exact nature of the pain.
- Where in the knee is your pain?
- What does the pain feel like?
- How long has the pain been present?
- Has it happened before?
- Describe any injuries to the knee.
- What makes it better or worse?
- Does the knee pain wake you up at night?
- Does the knee feel unstable?
- Have you been limping?
Your therapist will also want to know a bit about you.
- Do you have any major medical problems?
- How active is your lifestyle?
- What are the names of the medications you are taking?
Your therapist will want to know about any related symptoms.
- Do you still have normal sensation in your feet and lower leg? If not, this may be a more serious injury and requires immediate attention.
- Have you been having fevers?
Physical exam
- Your highly skilled physiotherapist will likely have you in shorts to completely expose the knee. If possible, wear shorts to your appointment.
- Your therapist will then inspect the knee and press around the knee to see exactly where it is tender. Your manual therapist will perform a number of maneuvers to stress the ligaments, tendons, and menisci of the knee and evaluate the integrity of each of these. At Physioactive, your physical exam doesn’t stop at the knee. Your therapist will look at your back, hips, ankles and feet to determine what contributing factors could be at play predisposing you to your injury and pain. This can sometimes be more important for successful treatment of knee pain, especially if related to overuse to pain that begins with no specific injury.
Using medical imaging to confirm our diagnosis. Our physiotherapists are trained to make an accurate diagnosis of your knee problem. We will work with your doctor and use medical imaging such as X-rays, CT scans, and other tests to support our impression. Research has been shown that frequently these imaging tests may not be relevant to your condition and can negatively impact your recovery.
- Depending on your particular history and exam, your doctor may suggest X-rays of the knee. X-rays show fractures (broken bones) and dislocations of bones in the knee. We can also see changes in joint space. Rarely, the doctor may order a CT Scan (a 3-dimensional X-ray) of the knee to precisely define a fracture or deformity.
- Both X-rays and CT scans are excellent for diagnosing fractures. They both are also poor, however, at evaluating soft tissue structures of the knee such as ligaments, tendons, and the menisci. Your therapist will use these tests to confirm their clinical impression.
MRI
- Magnetic resonance imaging (MRI) uses large magnets to create a 3-dimensional image of the knee.
- In contrast to CT scans, MRIs do not image bones and fractures as well.
- Also in contrast to CT scans, MRIs are excellent for evaluating ligaments and tendons for injuries. In most instances therapy can be started without an MRI. In most cases an MRI will not change how your physiotherapy will be progressed. It is important to continue your therapy while waiting for your MRI in most cases.
Common Symptoms of Knee Pain
At PhysioActive our unique coordinated approach has been shown to be the most effective in pain relief, strength, range of motion, and functional optimization.
The nerves that provide sensation to the knee come from the lower back and also provide hip, leg, and ankle sensation. Pain from a deeper injury (called referred pain) can be passed along the nerve to be felt on the surface. Knee pain, therefore, can arise from the knee itself or be referred from conditions of the hip, ankle, or lower back. All of the following sources of knee pain arise from the knee joint itself.
In general, knee pain is either immediate (acute) or long-term (chronic). Acute knee pains can be caused by an acute injury or infection. Chronic knee pain is often from injuries or inflammation (such as arthritis) but can also be caused by infection.
Acute Knee Pain
Meniscal Injuries
- Description: Injuries to the meniscus are typically traumatic injuries but can also be due to overuse. Often, a piece of the meniscus will tear off and float in the knee joint.
- Symptoms: Meniscal injuries may cause the knee to lock in a particular position, or either click or grind through its range of motion. Meniscal injuries may also cause the knee to give way. Swelling typically accompanies these symptoms although the swelling is much less severe than with an ACL injury.
- Treatment: Meniscal injuries often require arthroscopic surgical repair. A locking knee or a knee that “gives” should be evaluated for arthroscopic repair.
ACL Injuries
Sprained and Torn Cruciate Ligaments – We hear about this a lot on the sporting news and several of our Physioactive PT’s have injured them too. Now Connor McDavid is in the news and has proven that our principles at Physioactive can be achieved. Conservative rehabilitation success!
Athletes, as well as members of the general population, injure their anterior cruciate ligament (ACL) more than any other ligament. The exact reason is hard to pin down, but at Physioactive we have seen a pattern of weak core, hips, and feet to name a few deficits our clients present with. We do know that around 50% of athletes who suffer an ACL tear never return to the same level of play according to research(1). In addition, nearly one-third of those that do return to the sport go on to suffer a repeat tear(1). At Physioactive, we look at these contributing factors and our clients seem to buck this trend.
- Description: An anterior cruciate ligament (ACL) injury is a common sports injury generally caused by a hard stop or a violent twisting of the knee. The posterior cruciate ligament (PCL) is stronger than the ACL and much less commonly torn. The PCL requires strong forces, such as those produced when the dashboard strikes the knee in a car accident, to tear. Due to these severe forces, PCL injury is often associated with other ligament and bone injuries.
- Symptoms: If you tear your ACL, you may hear a pop. You may also notice your knee gives way or become unstable. At the time of injury, shock may set in and many of our clients feel nauseous at the time of injury. This will, almost always, be followed by marked knee swelling over the next couple of hours because the ACL bleeds briskly when torn.
- Treatment: Surgical repair is frequently recommended for high-level athletes who demand optimal outcomes especially in contact sports. Emerging research (2) and now proof (Thanks Conner McDavid) shows that conservative treatment and knee braces may prove sufficient for those committed to their rehab. Clinical signs of no instability will significantly increase this likelihood.
Tendon Ruptures
- Description: Less common. Both the quadriceps and patellar tendons may rupture partially or completely. A quadriceps tendon rupture typically occurs in recreational athletes older than 40 years or patellar tendon rupture typically occurs in younger people who have had previous tendonitis or steroid injections to the knee.
- Symptoms: Rupture of either the quadriceps or patellar tendon causes pain (especially when trying to kick or extend the knee). Those people with complete ruptures are unable to extend the knee. The patella is also often out of place either upward (with patellar tendon rupture) or downward (with quadriceps tendon rupture).
- Treatment: Tendon ruptures should be evaluated urgently. Tendon ruptures generally require surgical repair. A partial rupture may be treated with splinting alone.
Dislocated Kneecap (patella)
- Description: A common injury caused by direct trauma or forceful straightening of the leg, such as an injury that happens when serving in volleyball or tennis. Kneecap dislocation is more common in women, the obese, knock-kneed people, and in those with high-riding kneecaps.
- Symptoms: If you have this injury, you will notice the patella being out of place and may have difficulty flexing or extending your knee.
- Treatment: The doctor will move the patella back into place (reduce the dislocation). Even if the patella goes back into place by itself, however, it needs to be X-rayed for a fracture. After reducing the patella and ensuring the absence of a fracture, the doctors will treat these injuries by splinting the knee for 3 weeks to allow the soft tissues around the patella to heal followed by strengthening exercises to keep the patella in line. This injury often causes damage to the cartilage on the back of the patella.
Bursitis
- Description: As a result of trauma, infection, or crystalline deposits, the various bursae of the knee may become inflamed.
- Symptoms: Acute or chronic trauma causes a painful and often swollen knee from the inflammation of the bursae. A particular common bursitis is prepatellar bursitis. This type of bursitis occurs in people who work on their knees. It is often referred to as a carpet layer’s knee. Another type of bursitis is pes anserine bursitis. The anserine bursa is located about 2 inches below the knee along the medial side of the knee. More commonly occurring in the overweight and in women, but also affecting athletes and others, anserine bursitis often causes pain in the region of the bursa and is often worse with bending the knee or at night with sleep.
- Treatment: Treatment will usually include home care with PRICE therapy and NSAIDs. Severe forms, however, can be treated with periodic steroid injections to the
Jumper’s Knee
- Description: Tendonitis (inflammation of the tendon) of the quadriceps tendon at the upper point of the patella, where it inserts, or tendonitis of the patellar tendon either at the lower point of the patella or at the place where it inserts on the tibia (called the tibial tuberosity, the bump about 2 inches below the knee on the front side), is termed jumper’s knee. Jumper’s knee is so named because it is typically seen in basketball players, volleyball players, and people doing other jumping sports.
- Symptoms: Jumper’s knee causes localized pain that is worse with activity. It usually hurts more as you jump up than when you land because jumping puts more stress on tendons of the knee.
- Treatment: Home therapy with the PRICE regimen together with anti-inflammatory drugs is the basis of treatment. Particularly important are rest, ice, and NSAID drugs, which will help stop the pain and break the cycle of inflammation. After controlling the pain, you should slowly start an exercise regimen to strengthen the quadriceps and hamstring muscles and resume your sport of choice a few weeks down the line. Also, bracing of the extensor mechanism may help remove stress from the tendons.
Osgood-Schlatter Disease
- Description: Osgood-Schlatter disease occurs in adolescent athletes where repetitive extension of the knee causes inflammation and injury of the tibial tubercle (the bony protrusion at the top of the shin, just below the kneecap).
- Symptoms: Children suffering from this syndrome report pain and swelling at the tibial tubercle. This pain is typically worse when extending the leg. The tibial tubercle is tender to touch and over time begins to protrude more because the chronic inflammation stimulates the bone to grow.
- Treatment: Osgood-Schlatter disease is a self-limited condition that usually resolves as the tibial tubercle stops growing with the end of adolescence (at about age 17 years in males and age 15 years in females). It frequently occurs during periods of rapid growth. At Physioactive we find that overuse of one of the quads is frequently the key to successful long term results. Acute treatment includes PRICE and NSAID therapy. In severe cases, splinting the knee for a few weeks may help reduce the pain and halt the inflammation cycle.
Patellofemoral Syndrome and Chondromalacia Patella
- Description: These 2 conditions represent a spectrum of disease caused by patellar maltracking.
- Symptoms: The condition typically occurs in young women and also in athletes of both sexes and elderly people. In patellofemoral syndrome, the patella rubs against the inner or outer femur rather than tracking straight down the middle. As a result, the patellofemoral joint on either the inner or outer side may become inflamed causing pain that is worse with activity or prolonged sitting. As the condition progresses, softening and roughening of the articular cartilage on the underside of the patella occurs, and the syndrome is referred to as chondromalacia patella.
- Treatment: Home care with PRICE therapy, NSAIDs, and exercises (such as straight leg raises) that balance the muscles around the patella work for most people. Others may benefit from bracing or taping of the patella, commercial arch supports (for the arch of the foot), or orthotic supports that correct foot mechanics and may reduce abnormal forces on the knee. Severe cases of patellofemoral syndrome or chondromalacia may be treated surgically through a variety of procedures.
Knee Pain Prevention
Knee pain has a host of causes. Many types of pain are difficult to prevent, but you can do some general things to reduce the likelihood of sustaining a knee injury.
Stay Slim
- Staying slim reduces the forces placed on the knee during both athletics and everyday walking and may, according to some medical research, reduce osteoarthritis.
- Keeping your weight down may also reduce the number of ligament and tendon injuries for similar reasons.
Keep Limber, Keep Fit
- Many knee problems are caused by tight or imbalanced musculature. Stretching and strengthening, therefore, also help to prevent knee pain.
- Stretching keeps your knee from being too tight and aids in preventing both patellofemoral syndrome and iliotibial band syndrome.
- Strengthening exercises particularly of the quadriceps (straight leg raises and leg extensions are two excellent exercises, but please see a book on exercise and training for more) can help prevent knee injury.
Exercise Wisely
- If you have chronic knee pain, consider swimming or water exercises.
- In water, the force of buoyancy supports some of our weight so our knees do not have to.
- If you don’t have access to a pool or do not enjoy water activities, at least try to limit hard pounding and twisting activities such as basketball, tennis, or jogging.
- You may find that your aching knees will act up if you play basketball or tennis every day but will not if you limit your pounding sports to twice a week.
- Whatever you do, respect and listen to your body. If it hurts, change what you are doing.
- If you are fatigued, consider stopping — many injuries occur when people are tired.
Protect the Knee
- Wearing proper protection for the activity at hand can help avoid knee injuries.
- When playing volleyball or when laying carpet, protecting your knees may include kneepads.
- When driving, knee protection may include wearing a seatbelt to avoid the knee-versus-dashboard injuries as well as injuries to other parts of your body.
Chronic Knee Pain
Arthritis: Arthritis of the knee is an inflammatory disorder of the knee joint that is often painful. Arthritis has many causes.
Knee Osteoarthritis
- Description: Osteoarthritis (OA) is caused by the degeneration of cartilage in the knee. In its extreme form, the menisci (cartilage) will be completely eroded, and the femur will rub on the tibia, bone on bone.
- Symptoms: Osteoarthritis can cause a chronically painful knee that is usually more painful with activity.
- Treatment: Treatment is aimed at pain control with over-the-counter pain relievers. Anti-inflammatory medications, either over-the-counter or by your doctor’s prescription, are also quite helpful. More severe OA can be treated with narcotic pain medicines or a knee joint replacement. Most clients do well with conservative treatment, increasing range, strength, and movement. All of our clients that have attended our prehabilitation program have gone on to postpone or cancel their total knee surgeries as they did so well with their therapy.
Rheumatoid Arthritis of the Knee
- Description: Rheumatoid arthritis (RA) is a connective tissue disease of the whole body that affects many joints often including the knee. People who have this disease often have family members who suffer from it as well.
- Symptoms: In addition to knee pain, rheumatoid arthritis may produce morning stiffness and pain in other joints.
- Treatment: Treatment includes pain medications, anti-inflammatory medications, and prescription drugs (such as methotrexate) that assist in controlling the body’s abnormal immune response and can slow disease progression.
Crystalline Arthritis (gout and pseudogout)
- Description: These severely painful forms of arthritis are caused by sharp crystals that form in the knee and other joints. These crystals can form as a result of defects in the absorption or metabolism of various natural substances such as uric acid (which produces gout) and calcium pyrophosphate (pseudogout).
- Treatment: Treatment is aimed at controlling inflammation with anti-inflammatory medications, and at aiding the metabolism of the various chemicals that may lead to crystal formation.
Infection (or sometimes called infectious arthritis)
- Description: Many organisms can infect the knee. Post injection or infections such as Gonorrhea, a common sexually transmitted disease, can infect the knee, as can common organisms residing on your skin.
- Symptoms: Infection of the knee causes painful knee swelling. In addition, people who develop such infections typically complain of fevers and chills. Less severe infections may not have associated fevers or cause this ill-feeling.
- Treatment: New swelling and pain in the knee should be evaluated for infection especially if there is no mechanical cause for the swelling. Your therapist is well versed in this and will refer you to your physician for their opinion if appropriate. Treatment usually includes intensive antibiotic therapy and may include aspiration of the joint, or surgical drainage of the infection.
Iliotibial Band Syndrome
- Description: A fibrous ligament, called the iliotibial band, extends from the outside of the pelvic bone to the outside of the tibia. When this band is tight it may rub against the bottom outer portion of the femur (the lateral femoral condyle).
- Symptoms: Distance runners typically suffer from this condition. These runners complain of outside knee pain usually at the lateral femoral condyle. Early on, the pain will typically come on 10 minutes to 15 minutes into a run and improve with rest.
- Treatment: Local treatment of the iliotibial band syndrome is to release, stretch and mobilize the iliotibial band. Self foam rolling and cupping can also be effective. At Physioactive, we most commonly see a foot or hip/core weakness leading to overuse of TFL, gluts and quads leading to more tension in the ITB. In addition to stretching the iliotibial band, PRICE therapy and NSAIDs may be of some help.
Don’t Settle
We have a record of treating even the most complicated knee conditions as well as post-operative knee surgeries, or simple sports injuries. Regardless of how debilitating your pain is, or how long you have suffered from your condition, we are committed to trying every tool in our chest to get you feeling better and back to your life.
When you deal with chronic pain, it’s easy to forget how much you enjoyed life before the pain became your constant companion. Because the onset of chronic pain is often slow and steady, you may feel hopeless about the future and can’t imagine a time that you were free from pain. At PhysioActive, we provide you with the physical solutions and the emotional and mental support you need to commit yourself to rid your body of chronic pain.
Schedule an Appointment Today
Schedule an appointment today by calling 905-695-0371 or filling out our simple online request form. When you visit our clinic, you’ll find a group of professionals that are committed to helping you find solutions for better health and wellness and a future that is bright and exciting. Please make sure to tell the office staff why you are booking and the will direct you in the right direction.